Facing Infertility: Your Options For Parenthood (Also, You’re Not Alone)
The World Health Organization has now classed infertility as a disease and a global health burden with consequences for mental health, economic deprivation, social isolation, and reproductive health rights.
The reasons for infertility and fertility issues can be quite complex and sometimes unknown. Unfortunately, women shoulder a disproportionate amount of the blame for fertility issues, under the incorrect assumption that since she carries and bears the child, she must have the greatest effect on fertility. However, statistics show that within a couple, the contributing factors to infertility break down as follows¹:
up to 50% of infertility cases are due to the female
20-30% due to the male
20-30% is a combination of factors between both the man and the woman, with a percentage of cases being “unexplained infertility”
The stigma attached to the inability to become pregnant or have a child can be strong, particularly in developing countries. It can lead to women being ostracized, shunned from their communities, or being denied participation in family and community traditions. It can be used as grounds for divorce or justification for why a girl is not considered marriageable and then a burden to her family, community, or society. This rejection from your family and community can understandably lead to mental health issues and even suicide.
Fertility also raises issues of reproductive health and human rights. This is especially emphasized in countries such as South Africa, Namibia, Chile where it’s been found that women who were HIV-positive were being sterilized without their knowledge and without their consent². Women may believe they are having fertility issues for other reasons when in reality they were sterilized during a previous procedure and not informed of what was happening.
But the stigma is not limited to developing countries. Many women and couples in developed countries with fertility issues have experienced the curiosity of friends of family asking “are you going to have children?” without even thinking about the emotions that question can raise.
And while the conversation around “we’re trying for a baby” can be difficult enough when it doesn’t seem to be happening, “we’re doing IVF” can evoke another set of reactions and stigma.

Who needs access to fertility treatments?
The term “fertility treatments” or assisted reproduction now encompasses several different types of treatments, such as in vitro fertilization, egg donation, sperm donation, artificial insemination, embryo donation and adoption.
Those with infertility or fertility issues will be the largest group seeking access to fertility treatments, yet access also poses an issue for those that need assistance to conceive a child such as same-sex couples, single women or men, people with genetic disorders, and couples older than the age restriction imposed in some countries.
Also, for women who have been involuntarily sterilized through a tubal ligation or had their “tubes tied”, a tubal ligation reversal may not be sufficient to allow them to conceive naturally again. In vitro fertilization (IVF) can be a viable option for women who have had this procedure.
The IVF process is generally the longest, most expensive, and emotionally taxing of the fertility treatments available. Currently, the success rate for IVF worldwide is about 30%, although this rate can differ by clinic. But for couples who have been trying to conceive for more than 1 year without success (6 months if the woman is over 35) or those that need assistance to conceive, it provides some hope of being able to give birth to a child.
However, if you have been experiencing infertility or fertility issues, diagnosis of the reason or reasons for the infertility is key to giving you the best shot of having a successful IVF cycle.
Diagnostics & testing
There are several tests that can be conducted to investigate why you’re experiencing infertility. Non-invasive testing will be conducted first by taking a detailed medical histories from you and your partner; conducting blood tests to evaluate hormone levels, look for viruses or infections or and/or conduct chromosomal genetic testing; and a semen analysis for men.
If none of those tests reveals an obvious reason for the infertility, then more invasive tests can be conducted to visually look for physical abnormalities or obstructions in the woman’s uterus, cervix, and fallopian tubes.
As mentioned earlier, a small percentage of infertility is considered “unexplained” when no obvious reason can be found through the standard diagnostics and tests.
Going through proper diagnosing and testing may allow you to find a reason for your infertility and resolve it, thus allowing you to conceive naturally. Or testing may reveal a diagnosis showing that natural conception is difficult or not possible and IVF will your best shot at conceiving a child. If that’s the case, here’s what you can expect when going through in vitro fertilization.
Who needs access to fertility treatments?
The term “fertility treatments” or assisted reproduction now encompasses several different types of treatments, such as in vitro fertilization, egg donation, sperm donation, artificial insemination, embryo donation and adoption.
Those with infertility or fertility issues will be the largest group seeking access to fertility treatments, yet access also poses an issue for those that need assistance to conceive a child such as same-sex couples, single women or men, people with genetic disorders, and couples older than the age restriction imposed in some countries.
Also, for women who have been involuntarily sterilized through a tubal ligation or had their “tubes tied”, a tubal ligation reversal may not be sufficient to allow them to conceive naturally again. In vitro fertilization (IVF) can be a viable option for women who have had this procedure.
The IVF process is generally the longest, most expensive, and emotionally taxing of the fertility treatments available. Currently, the success rate for IVF worldwide is about 30%, although this rate can differ by clinic. But for couples who have been trying to conceive for more than 1 year without success (6 months if the woman is over 35) or those that need assistance to conceive, it provides some hope of being able to give birth to a child.
However, if you have been experiencing infertility or fertility issues, diagnosis of the reason or reasons for the infertility is key to giving you the best shot of having a successful IVF cycle.
Diagnostics & testing
There are several tests that can be conducted to investigate why you’re experiencing infertility. Non-invasive testing will be conducted first by taking a detailed medical histories from you and your partner; conducting blood tests to evaluate hormone levels, look for viruses or infections or and/or conduct chromosomal genetic testing; and a semen analysis for men.
If none of those tests reveals an obvious reason for the infertility, then more invasive tests can be conducted to visually look for physical abnormalities or obstructions in the woman’s uterus, cervix, and fallopian tubes.
As mentioned earlier, a small percentage of infertility is considered “unexplained” when no obvious reason can be found through the standard diagnostics and tests.
Going through proper diagnosing and testing may allow you to find a reason for your infertility and resolve it, thus allowing you to conceive naturally. Or testing may reveal a diagnosis showing that natural conception is difficult or not possible and IVF will your best shot at conceiving a child. If that’s the case, here’s what you can expect when going through in vitro fertilization.
In Vitro Fertilization: Step-by-Step
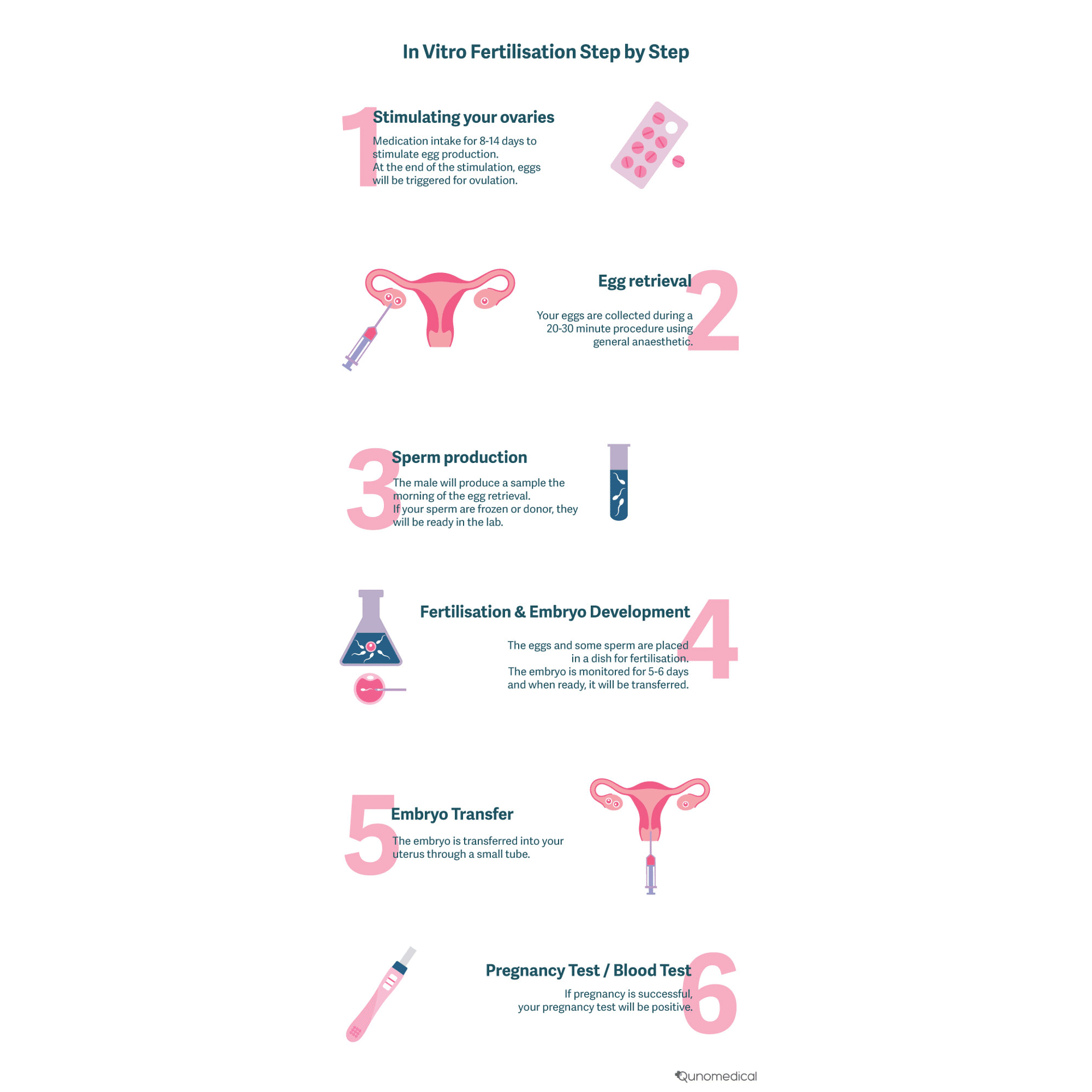
1. Stimulating your ovaries
The first day of your period will technically be the start of your IVF cycle, however, you will wait until day 2 or 3 to start your hormone injections.
You’ll take medication, usually in the form of injections, to encourage the follicles in your ovaries to produce more eggs so there are enough to harvest. Typically, it will be 2 injections per day (1 in the morning and 1 in the evening).
You may be monitored by ultrasound around day 8 to ensure that the eggs are developing. Towards the end of the stimulation you will get a “trigger injection”. This gets the eggs ready for ovulation – the natural process where eggs are released and you have your period. You will be told exactly when to administer the trigger injection. Shortly after this, your egg retrieval will happen.
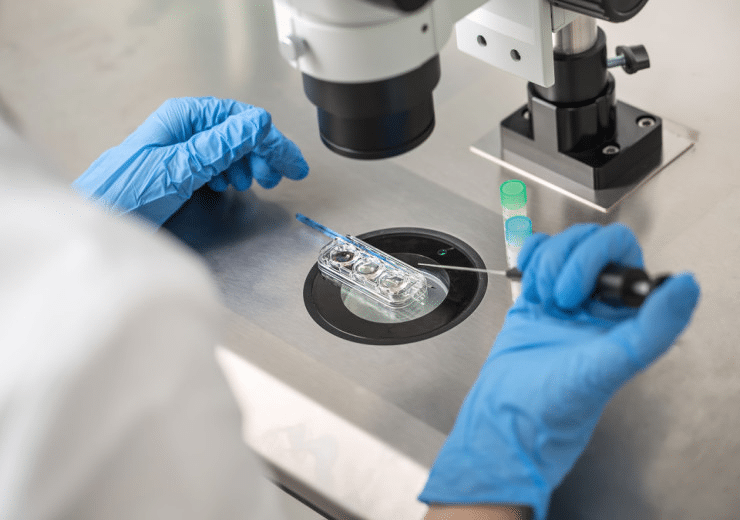
2. Egg Retrieval
This is a short, out-patient procedure where your eggs are collected from your ovaries. You’ll be under general anaesthesia and the procedure takes about 20-30 minutes. Using ultrasound technology, a needle is guided into each ovary.
It’s delicate work where every millimetre counts, and needs to be done by a specialist. Your eggs are contained in the fluid within the follicles in your ovaries and are not visible with the naked eye. Instead, the fluid that looks like it contains a developed egg is removed from the follicles.
Ultrasounds before the retrieval should give your specialist a good idea of how many eggs can be collected. The average number collected is 8-15 eggs.
Your recovery should be about 30 minutes and you’ll be able to leave the office that day, but you should have someone pick you up since you were under general anaesthesia.
3. Sperm Production
The male will need to produce a sperm sample on the morning of the egg retrieval. If the sperm was previously frozen or donor, the sample will be ready in the lab.
4. Fertilisation & Embryo Development
The eggs and some sperm will be placed in a dish (in vitro). There, they will have the chance to find each other and fertilize like they would naturally in the body.
The embryos are put into a special incubator where the conditions for growth and development are perfect. The embryos are monitored for 5-6 days and when they are ready, they will be transferred to the uterus.
5. Embryo Transfer
If the embryo or embryos develop in the lab, they are ready to be transferred into your uterus. The embryo transfer is a very simple process, similar to a pap smear.
The embryos are placed into a small tube called a catheter. It is critical that the embryo is disturbed as little as possible so this step should be done by an expert. Your fertility specialist then places the catheter through your cervix and into your uterus and the embryos are deposited into your uterus.
The procedure should take about 5 minutes and is done without any anaesthesia so you will be awake. You will be able to get up shortly after and continue with your day. There is no concern that the embryos will fall out if you stand up or go to the toilet.
Even though you can get on with your day, it is best to try to relax and take it easy. You want to have the best conditions for the embryo to implant in your uterus, so try to eliminate all stress during the “2-week wait” when the embryos will be implanting.
Many patients are also provided with progesterone to administer into the vagina for around 10 days to help achieve maximum chance of success for implantation.
It is possible that some light bleeding may happen during this time that can be confused with your period. This can be normal and is called “implantation bleeding.” There is generally no reason to be worried but inform your doctor if the bleeding becomes heavy.
6. Pregnancy Test / Blood Test
You can take a pregnancy test 10-14 days after the embryo transfer. It is best to not take a home pregnancy test, but rather wait for the blood test at the clinic.
This is because the level of hormones in your body is still very high and can yield false results through urine tests. Blood test is best!
What if you want to have IVF abroad?
The typical timeframe of an IVF cycle is around 6 weeks. This doesn’t mean you have to spend 6 weeks away from home. Below are a few indications on how to make your IVF journey abroad easier.
Tests you can take at home that can be sent to IVF specialists abroad:
Female: Rh blood group, Complete blood count (CBC), Glucose + creatinine + urea, International Normalized Ratio (INR), HIV, HCV, HBsAg, sífilis v.d.r.l, Toxoplasma IgG, Rubella IgG, Antimullerian hormone
Male: Rh blood group, HIV, HCV, HBsAg, sífilis v.d.r.l, Seminogram
Female: Ultrasound
First consultation with your patient manager (can be done remotely)
This consultation is possible to find out information about the operational side of the treatment, e.g. what treatments are offered or how it can be organised. It does not involve the doctor and is non-medical.
Second consultation with the doctor (can be done in person or remotely)
If you have your diagnostics and test results, the clinic will invite you to a consultation to discuss your results and treatment options.
At home or abroad? IVF steps in detail
Once you decide to go ahead with your treatment, you will start with the IVF procedure as described above. Also in this case, there are a few steps that can be done at home. Here’s a rundown:
1. Ovarian stimulation: Can be done in person or distance - for distance: The clinic can prescribe you the medication that you purchase locally and administer at home. 2. Egg retrieval: Needs to be done at the clinic 3. Sperm production: Needs to be done at the clinic 4. Fertilization & embryo development: Needs to be done at the clinic 5. Embryo transfer: Needs to be done at the clinic 6. Pregnancy test: In order to know if IVF was successful, you’ll need to take a blood test, which you can also do at your local practice. So while the whole process is about 6 weeks long, you will need to physically be at the clinic for egg retrieval, fertilization and embryo transfer, which will take approximately 7 to 10 days, depending on the clinic and your individual needs.
Unused Eggs/Embryo
In the case that you produce excess eggs or more viable embryos result than are implanted, you can freeze them for future use. This usually incurs an extra cost. The legal guidelines for egg and embryo freezing duration vary from country to country.
Empowerment is key
Fertility is an issue that affects everyone. Whether you suffer from infertility, are able to have children or even decide not to have children. No one should be made to feel ashamed or shunned for a journey that is sometimes beyond their control. By helping to shed light on the fertility process and contributing to the global conversation, we are here to say you are not alone.
Sources
Find the Right Specialist at a Fraction of the Cost
Qunomedical only lists clinics and doctors that have been thoroughly vetted with quality and affordability in mind. Contact us for your 100% free, non-binding assessment.

Patient manager
Frieda
Your personal Patient Manager
Let's talk
Still unsure? Feeling overwhelmed? Talking to a real person can give you the guidance and reassurance needed. You don’t have to do it alone. Let’s find the right doctor together.